
Although most textbooks focus on the velopharyngeal part of this system, this chapter covers the complete velopharyngeal-nasal apparatus as a single functional entity. The velopharyngeal-nasal apparatus is located within the head and neck and comprises a system of valves and air passages that interconnects the pharynx (throat) and the atmosphere through the nose. 2015 272(8):2035–8.Velopharyngeal-Nasal Function and Speech Production An algorithm for treating extracranial head and neck schwannomas. Yafit D, Horowitz G, Vital I, Locketz G, Fliss DM. Parapharyngeal space tumors: the infratemporal fossa approach. Tumors and surgery of the parapharyngeal space.
#Superior constrictor muscle attachment series
Histopathologic classification of parapharyngeal space tumors: a case series and review of the literature. Locketz GD, Horowitz G, Abu-Ghanem S, Wasserzug O, Abergel A, Yehuda M, Fliss DM. Surgical management of parapharyngeal space tumors: a 10-year review.
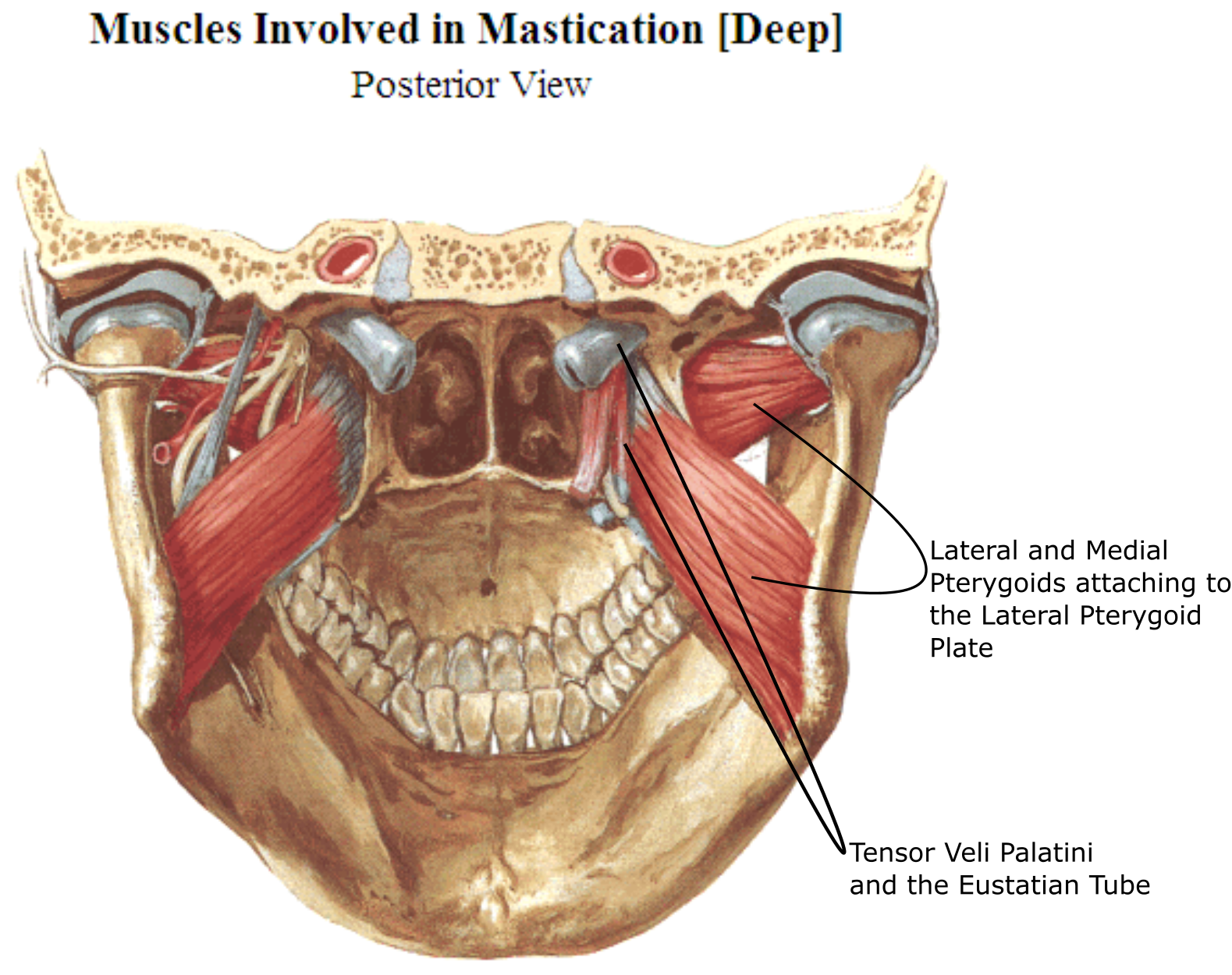
Khafif A, Segev Y, Kaplan DM, Gil Z, Fliss DM. The transcervical approach for parapharyngeal space pleomorphic adenomas: indications and technique. Horowitz G, Ben-Ari O, Wasserzug O, Weizman N, Yehuda M, Fliss DM. Surgical management of parapharyngeal space masses. Management of tumors arising in the parapharyngeal space. This chapter describes the common surgical approaches to the PPS. The anatomical extent of the tumor, its histologic type (benign or malignant), and the patient’s medical history (previous surgeries or radiation treatment) determine the surgical approach. Standard surgical approaches to the PPS include the transcervical approach, the transparotid-transcervical approach, the transmandibular approach, the endoscopic transnasal approach, the transoral robotic surgery, and the infratemporal fossa approach. Symptoms include change in voice, trismus, mass in the upper neck, cranial nerve deficits, serous otitis media (due to Eustachian tube obstruction), and obstructive sleep apnea. In addition, the radiological evaluation of any patient with suspected malignancy must include the neck, to evaluate for lymph node metastasis. Perineural invasion is common in adenoid cystic carcinoma and is the pathway to the intracranial space, so imaging studies should be directed toward the foramen ovale, foramen rotundum, cavernous sinus, orbital apex, trigeminal ganglion, and dura.
Hematogenous or lymphatic spread can also occur, as well as perineural invasion along cranial nerves. Malignant tumors arising in the PPS can invade the intracranial compartment, maxilla, mandible, temporomandibular joint, orbit, or skin. Pleomorphic adenoma is the most common benign tumor of the PPS, followed by schwannomas and paragangliomas. Tumors can originate in the PPS or can invade the space from neighboring areas. The PPS can harbor tumors and infectious processes, but both infectious processes and neoplasms are rare. Its borders include the nasopharynx and oropharynx medially, the masticator space anterolaterally, the deep lobe of the parotid gland posterolaterally, and the retropharyngeal space posteromedially. The parapharyngeal space (PPS) is a potential space between the skull base above and the hyoid bone below.


 0 kommentar(er)
0 kommentar(er)
